A huge crisis has been created in the insurance and health service industries due to the aging population of America. The number of patients has outnumbered the meager number of nurses, doctors and medical professionals available in the country. This has induced the country’s federal government to create better incentives for attracting more people towards these respective industries. Although a college or medical degree is required to be eligible for the majority of the jobs in these industries, you can apply for other supporting jobs, such as coding specialists and medical billing specialist. These jobs are escalating at an increasing speed of more than 20 percent per year.
How Much Do Medical Coders Make?
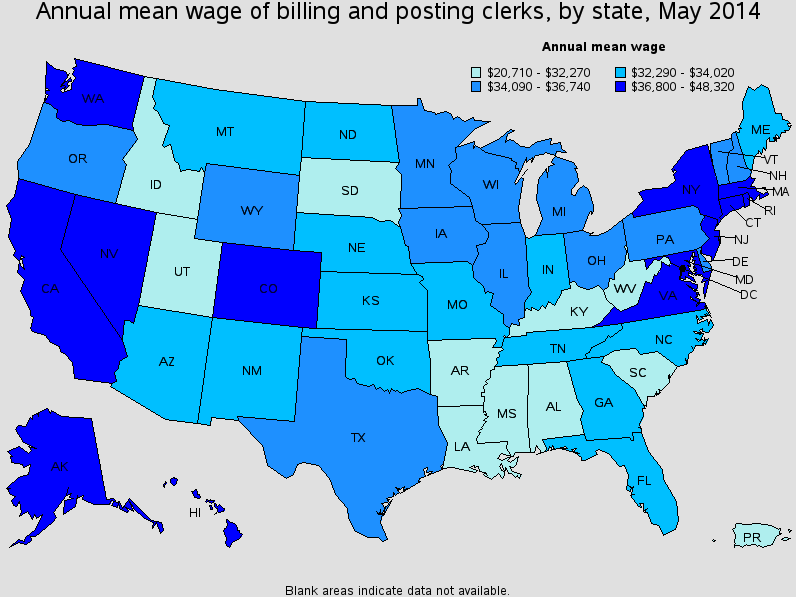
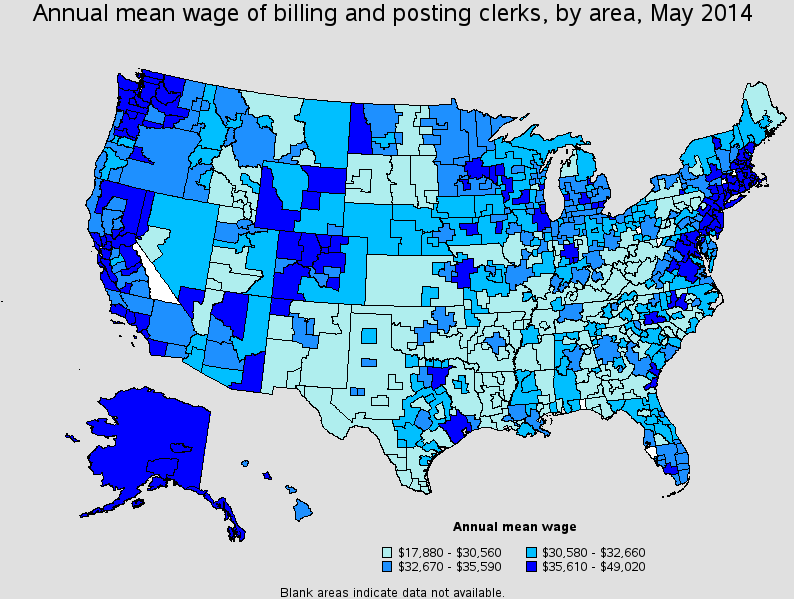
The wages and salaries for medical coders tend to increase every year due to the hefty demand for medical coders. According to the most recent reports provided by the Bureau of Labor Statistics, medical coders make about $16.42/ hour on average and enjoy an annual wage of approximately $34,160. The annual salary tends to vary from one location to another. The highest paid top ten earners of this industry make over $56,000/ year, while the earners in the bottom make a little over $22,000/ year. This profession does not even demand you to have a college degree, but still pays better than most of the career options available.
Professional medical coders work in professional office setting and are given generous packages that include health and medical benefits. To answer how much medical coders make, you should also know that the areas and facilities in which you work also make a difference, below is the data from bureau of labor statistics:
What Do Medical Coders Do?
To truly understand how much do medical coders make, you have to know what they do. The job responsibilities of the medical coding and billing specialists include the following:
- Organization and preservation of the patient records, information and databases. This enables the nurses and doctors to easily access the correct and complete information pertinent to patients quickly.
- Translating the doctor’s notes to proper, standardized notes. This enables the medical personnel to quickly understand a patient’s situation by looking at the succinct summary of the patient instead of going through the extensive patient details.
- Updating the patient’s records and treatment procedures. Coders need to update the patient’s file when they receive a certain treatment procedure. This helps them track the treatment and service quality provided to the patient.
- Communicating between the billing agencies and healthcare workers. A major problem in the medical profession is to transfer information from the healthcare professionals and personnel to the people responsible for handling money. With the help of standardized codes, the medical coders are able to conveniently communicate complicated treatment histories and diagnoses to the billing agencies. This enables the billing agencies to accurately charge the insurer or patient.
- A medical coder also audits and re-files appeals of all the rejected claims. They educate the providers about the coding procedures and recommend suitable application of the compliance and federal mandates to the providers. Additionally, they may serve as the advocates of the patients and providers in case any issues arise.
In addition to understanding these duties, you should know that medical coding and billing aren’t exactly the same. The medical biller and coder are often the same person in an organization, or they work quite closely together, but their professions are quite different from each other. The medical coder has to ensure that appropriate codes are assigned to different claims. The coders inspect different sources placed in a patient’s medical database to confirm the procedures that were implemented. The coder has to assign CPT® codes, HCPCS codes and ICD-9 codes to the procedures and treatments that were exercised, to give medical biller all the information required for processing the reimbursement claim and right by the concerned insurance agency.
How to Become a Medical Coder
After learning the answer to how much do medical coders make, if you want to become one, here's what's required:
Professional Backgroud
A great deal of training and education is required for becoming a skilled and professional medical coder. Detailed knowledge of medical terminologies and anatomy is needed to venture into this field. Moreover, a coder must be familiar with the various kinds of insurance regulations, plans, compliances as well as the critical coding cooks: HCPCS Level II, ICD-9-CM and CPT.
The field of medical coding has evolved a lot since new policies and coding methods such as the ICD-9-M, HCPCS and CPT codes have been introduced. Coders who had knowledge of the Volumes 1, 2 and 3 of the ICD-9-M need to convert to ICD-10-CM as well as ICD-10-PCS. Coders with a sound knowledge of ICD-9-CM can easily make this transition and professionals who do not have a basic understanding of ICD-9-CM won’t be able to grasp the ICD-10 conveniently.
Certified coders are those who have passed the different coding tests. They are fluent in the technical medical language and terminologies, and have a comprehension of the fundamentals of the medical physiology, anatomy and terminology. To become a certified CPC, medical coders must study a year as CPC-A (Certified Professional Coder Apprentice).
Skills and Ethics
Coding is a very detail-oriented and laborious work. The coders need to review all the charts and details of the patients for learning their diagnosis and itemizing all the services provided to them. In case any service is not attended to properly, the provider won’t receive any payment for that service. If a wrong code has been implemented by the coder, the provider would need to return the additional payment and might face some legal charges due to overbilling. Coders need to be aware of the new regulations of the field as codes are constantly changing.
Hospitals, private practices, nursing facilities, outpatient clinics, laboratories, ambulatory surgical facilities, mental health facilities and health agencies employ professional and certified medical coders. Medical coders and billers are employed when the essential healthcare services and facilities are provided by a medical facility. Once they have mastered the core skills, the professional medical coders often venture into other rewarding and successful careers.
