Healthcare professionals find that they very frequently have to manage constipation issues in patients. However, although constipation is a common problem, each patient requires their own specific nursing care plan for constipation. A thorough evaluation of the issue is necessary in order to identify and then treat the underlying cause of constipation. The poor habits that lead to constipation are not always obvious from conversations between nurse and patient. Therefore, nurses will need to be aware of clues as to what these are, and identify any poor habits that the patient is currently unaware of.
What Is a Nursing Care Plan?
A nursing care plan describes the actions that will be undertaken whilst the patient is being cared for, and is part of nursing practice. A care plan will usually be drawn up by licensed practical nurses (LPNs) and registered nurses (RNs) following a thorough evaluation of the patient’s medical history and current condition. Nurses then work with the patient to fulfil the goals and objectives outlined in the plan.
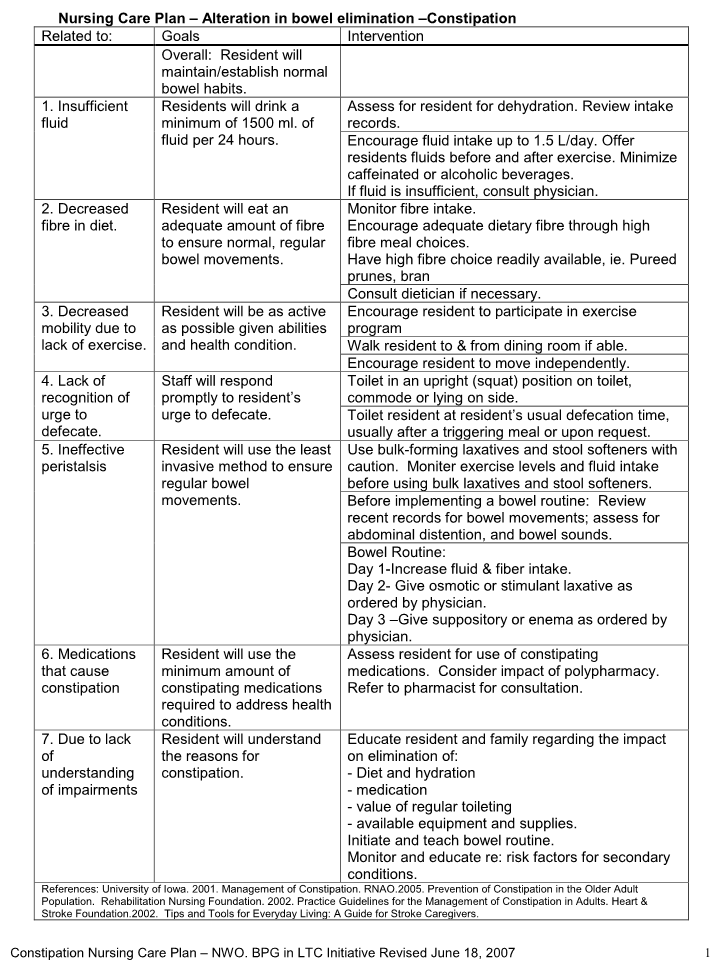
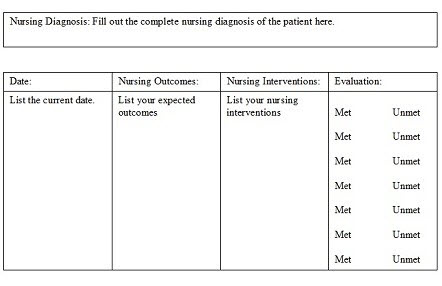
The design of the nursing care plan will vary between health care establishments. However, generally speaking, plans are categorized into four types: problem lists and nursing diagnoses, goals and criteria for outcome, nursing orders, and evaluation.
What to Consider in a Nursing Care Plan for Constipation
1. Determine Causative and Contributing Factors
- Review the patient’s daily diet.
- Evaluate fluid intake.
- Analyze the patient’s medication, and look at possible interactions or adverse effects.
- Talk to the patient about their laxative/enema usage, and look for signs of abuse.
- Assess the patient’s physical activity level.
- Determine potential stressors, be they financial, work-related, or personal.
- Go over the patient’s medical and surgical history.
- Assess the patient’s ability to care for themselves, along with their privacy and access to toilets.
- Ask if defecation hurts. Examine the patient’s perianal regions for fissures, hemorrhoids, skin breakdown, or other abnormalities.
- Look for fecal impaction.
- Palpate the abdominal area for masses or distention.
2. Assess the Usual Defecation Pattern
- Talk about their defecation issues, and their typical bathroom trip.
- Ask about what stimulates their bowel activity, and any interferences they have.
3. Evaluate the Current Defecation Pattern
- Write down the stool color, consistency, odor, quantity, and frequency. This provides a baseline, so any changes can be recognized.
- Ask the patient how long they have had their current issues, and their concerns.
- Listen for bowel activity by auscultating the abdomen.
- Find out if the patient is currently using laxatives or enemas.
- Review the patient’s current fluid and food intake.
4. To Aid a Return to an Acceptable Defecation Pattern
- Advise the patient how to incorporate fiber and bulk into their diet.
- Encourage the patient to drink lots of fluids, including fiber-rich fruit juices, and warm, stimulating drinks (such as tea and decaffeinated coffee) to promote soft, moist stool.
- Increase the patient’s levels of physical activity where possible to promote intestinal contractions.
- Schedule times for bathroom trips, and ensure the patient can defecate in private if possible.
- Provide any necessary medication, such as bulk-forming agents, stool softeners, and mild stimulants
- Apply a lubricant or anesthetic ointment to the patient’s anus if necessary.
- Provide enemas if they are needed. Digitally remove any impacted stool.
- Run the patient a bath in order to soothe the rectal area after defecation.
- When the patient has chronic or permanent dysfunction, establish a bowel program, including any necessary digital stimulation and glycerin suppositories.
5. Promoting Post-Hospital Health – Considerations upon Discharge
- Support the treatment of any underlying causes of constipation.
- Talk with the patient about underlying defecation physiology, and acceptable variations.
- Give information on the relationships between diet, fluid intake, exercise, and appropriate laxative usage.
- Discuss the reasons for interventions, and promote the continuation of any successful interventions.
- To assess the problem long-term, encourage the patient to keep an elimination journal.
- If the problem is recurring, outline specific actions the patient can take to gain some independence.
6. Documentation Focus
Assessment/Reassessment:
- Stool characteristics
- Underlying dynamics of defecation
- The patient’s usual bowel pattern and their current issues, how long they have persisted, and anything that may have contributed
Planning:
- A care/intervention plan, including any necessary lifestyle changes, and a list of those involved
- A teaching plan
Implementation/Evaluation:
- Record any responses to the interventions suggested in the nursing care plan for constipation and how they were implemented
- Any new changes to the stool and defecation patterns
- Note any progress toward the patient’s goals
- Any changes to the plan
Discharge planning:
- The patient’s individual long-term requirements, and who is responsible for any future actions
- How to perform follow-up care
- Any specific referrals made for the patient
For more about how to create a nursing care plan, please watch the video:
Samples of Nursing Care Plan for Constipation
Sample 1
Background:
A 27 year old woman has given birth via Caesarian section to a healthy baby girl three days ago and is in postpartum care. During and after the birth, she received multiple drugs. She says she is constipated and hasn’t had a bowel movement for five days. She has great trouble passing stools, and has to strain just to pass a hard small ball. Furthermore, she says that she feels a great pressure in her rectum, and the hemorrhoids she suffered towards the end of her pregnancy are giving her pain. This makes her scared to go to the bathroom.
Nursing diagnosis:
The nurses diagnose constipation with pain on defecation secondary to hemorrhoids. This is evidenced by the patient not having a bowel movement for five days, feeling rectal pressure, passing hardened stool, and suffering painful hemorrhoids.
Nursing interventions:
- To help with bowel function, the nursing administrator will administer Miralax and Colace under the guidance of a physician.
- Bowel function each day will be monitored and assessed.
- To ease the pain from hemorrhoids, topical creams and sitz baths will be provided.
- The patient will be taught three methods for keeping bowel movements regular.
- The patient will be educated on how to take her prescribed drugs for constipation.
Nursing objectives:
- That the patient will have a bowel movement before being discharged from hospital.
- The pain from her hemorrhoids will ease.
- She will verbalize three ways in which to keep her bowel movements regular.
- She will describe how to use her prescribed medications to prevent constipation.
Sample 2