Working as a nurse or caregiver of patients with tracheostomy means learning about the risks of infection or harm to patients. Tracheostomy suctioning is a sterile and delicate procedure. It is important to understand associated risks to prevent transfer of bacteria, harm delicate mucous membranes, or risk compromising oxygen levels in the patient.
Tracheostomies are one of the most common procedures seen in intensive care units, sub-acute units, and in homecare. There are around 100,000 tracheostomies done every year in the United States and almost every nurse will have some contact with a tracheostomy patient at some point in their career. Even family members and caregivers of tracheostomy patients need to learn proper care of the site and tracheostomy suctioning. Education on proper procedure can help prevent complications.
Why Is Tracheostomy Suctioning Needed?
 A tracheostomy is inserted to assist a person with breathing. It is a tube that passes into the airway at the level of the trachea. It completely bypasses the upper airway, which is usually the part of the airway that moistens, warms, and keeps the air clean. When someone has a tracheostomy, the airways can be exposed to irritants. As a natural protective measure, people with a tracheostomy tend to have more mucus production to keep the airway moist and free from contaminants. Suctioning helps to clear any excess mucus and contaminants. It is important to understand when to suction and when to leave a little mucus. If you suction too often, you may find more mucus production as a result.
A tracheostomy is inserted to assist a person with breathing. It is a tube that passes into the airway at the level of the trachea. It completely bypasses the upper airway, which is usually the part of the airway that moistens, warms, and keeps the air clean. When someone has a tracheostomy, the airways can be exposed to irritants. As a natural protective measure, people with a tracheostomy tend to have more mucus production to keep the airway moist and free from contaminants. Suctioning helps to clear any excess mucus and contaminants. It is important to understand when to suction and when to leave a little mucus. If you suction too often, you may find more mucus production as a result.
Tracheostomy is done on an “as needed” basis to prevent airway obstruction. Since every person is different in when they may need to “cough” and clear the airway, suctioning needs to be individualized according to needs rather than as part of the daily routine. Nurses and family caregivers need to be thoroughly trained on what to look for when a patient might need assistance with clearing the airway.
When to Do Tracheostomy Suctioning
Tracheostomy suctioning is done to clear excess mucus in a patient’s airways that may form into a mucus plug. Mucus plugs can cause a patient to have severe respiratory distress or even stop breathing. Sometimes it can be very clear that a patient needs suctioning, but other times it may be questionable. Here are some things to look at when deciding when to suction:
1) Do you hear mucus in the airway?
2) Has the patient just awakened for the day?
3) Will the patient be going to sleep soon?
4) Prior to eating
5) Prior to going outside
6) Does the patient seem to be breathing harder or faster?
7) Is the oxygen level dropping?
Just watch for constant increased secretions that last more than three or four days with a change in color. Secretions that are normal are clear to white in color. Constant mucus in the airways that comes out green, yellow, or tan may be cause for concern and the doctor should be notified.
Assessment Before Suctioning
Once you have determined a patient needs suctioning, it is important to run a quick assessment to make sure they will be able to tolerate the procedure. Always talk to the doctor and/or the respiratory therapist to ask for parameters i.e. oxygen level, number of respirations, heart rate, etc. Here are some important things to assess:
- Is the heart rate in an acceptable range? (Increased heart rate means the heart is having to work harder to oxygenate the body).
- Is the patient breathing faster than normal?
- What are the oxygen saturation levels?
- Are you having to turn up oxygen flow?
- Does your patient have a fever?
- What is the blood pressure?
- Skin color (check for blueness/cyanosis, pale skin)
If there is ever a question if a patient is stable enough for suctioning, contact the respiratory therapist that is assigned to the patient. If there are signs of severe respiratory distress, contact emergency medical help immediately.
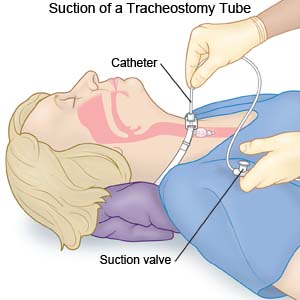
How to Do Tracheostomy Suctioning
After you have thoroughly assessed the patient, you will need to gather your supplies for suctioning.
You will need:
- Sterile suction catheter in a size that is right for the patient
- Sterile water
- Suction machine
- Connection tubing
- One clean, non-sterile glove
- Emergency Trach tube kit (In case trach tube becomes dislodged. You should also be trained in replacing a trach tube in an emergency or have a respiratory therapist close by)
Here is the procedure:
1) Wash your hands with soap and water.
2) Connect tubing to suction machine and turn machine on.
3) Place gloves on your hands.
4) Carefully open up just the end of suction catheter to expose connection.
5) Place connection of suction catheter onto tubing that goes to the machine. Keep catheter in package until ready to suction.
6) Place patient in a reclining position on their back.
7) Place a small amount of sterile water into the catheter to test suction.
8) Make sure only the inner cannula is out of the tracheostomy tube.
9) Place a few drops of sterile saline into the trach tube. Just a few tiny drops to thin the mucus.
10) Slowly insert the suction catheter into the tracheostomy and only go in around 4 centimeters.
11) Place your thumb over the vacuum button and slowly pull the catheter out as you “sweep” the trachea for mucus. Complete this step slowly, but within 5 to 10 seconds.
12) If more suctioning is needed, give your patient a few seconds to recover and repeat steps 1 through 11 without using anymore saline in the trach.
13) After the second pass, check your patient carefully again using the assessment steps above.
14) Clean suction catheter with a small amount of saline to rinse secretions out of tubing, then throw catheter away.
15) Replace patient’s inner cannula.
16) Turn off suction machine.
Step-by-step Tracheostomy Suctioning Instruction:
Tracheostomy Suctioning Risks and Precautions to Take
There are some risks associated with suctioning a tracheostomy. Some may only cause mild discomfort in the patient, but some may be life-threatening. Let’s take a look at the risks:
- Anxiety in the patient
- Low oxygen levels (Suctioning can suck some of the oxygen out of the airways. Ask a respiratory therapist if you can increase oxygen flow during suctioning. The catheter should always be left in LESS than 10 seconds and no longer.
- Tissue damage (Always keep the vacuum pressure turned to a low setting. This is normally around 60 to 150 mmHg, but always ask a respiratory therapist for clarification. If pressure is too high or the wrong catheter used, tissue damage can result).
- Infection (Suctioning is always a sterile procedure. Suction catheters should never be used more than once or rinsed in unsterile water. It is always best to use a “closed-suction” system to prevent the entry of bacteria into the respiratory tract).
