Antiglobulin test, also referred to as Coomb's test, is a frequently employed diagnostic tool that is used for the detection of immunohematological and immunological disorders. Based on the technique and objectives, there are two varieties of antiglobulin tests: the direct antiglobulin test (DAT)/direct Coomb's test (DCT), and the indirect antiglobulin test (IAT). It is imperative to mention that direct antiglobulin test is used to detect a special type of anemia that is caused by abnormal functioning of immune system. Human body is equipped to produce antibodies to identify and attack foreign pathogens. But in some cases, immune system synthesize antibodies that target and kill red blood cells (or RBCs in our body) to cause hemolytic anemia.
When Do You Need to Take a Direct Antiglobulin Test?
When your doctor is not sure if the antibodies are attached to your RBCs, direct antiglobulin test can help in such situation. Common scenarios where your doctor may recommend direct antiglobulin test include: post-transfusion indications of hemolytic anemia and sometimes diagnosing newborns if the mother has developed antibodies against fetal RBCs and passed it on to the baby during intrauterine life. If left undetected, the chances of developing life-threatening conditions like hemolytic disease of the newborn increases significantly.
Hemolytic anemias are usually due to hyperactivation of immune system that leads to the formation of antibodies against the body's own RBCs, which is also known as autoimmune hemolytic anemia. And symptoms may contain:
- Difficulty in breathing
- Lack of energy and increasing feeling of tiredness
- Dark colored urine and jaundice
- Low RBC count on the blood tests
- Cold extremities including hands and feet
- Heart issues like heart murmur or failure, and irregular heart
How Is the Direct Antiglobulin Test Performed?
Working Principle of DAT
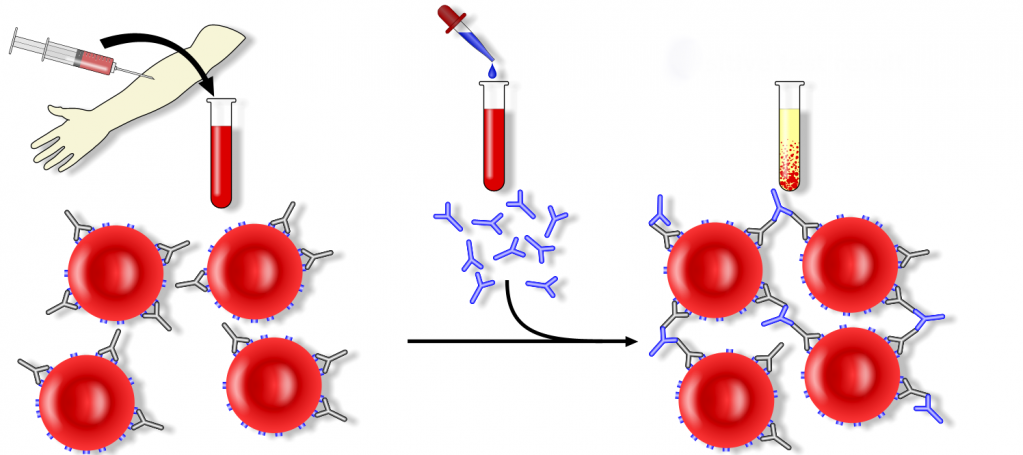
Direct antiglobulin test helps to detect the vivo antibody coating of your red blood cells (the antibodies could be IgG or compliment or both). In blood stream, RBCs have certain antigens that offer attachment sites to antibodies. Any trigger or response that can activate these attachment sites can stimulate the symptoms of hemolytic anemia. This is the basis of HDN (hemolytic disease of newborns), autoimmune hemolytic anemia and transfusion reaction. The activation and coating can also be caused due to certain medications.
In this test, red blood cells are washed and then incubated with human serum. This technique allows antibodies to get bind to the antigens on RBC. The process then involves washing and addition of anti-human globulin. If agglutination occurs after addition of anti-human globulin (sometimes referred to as Coombs reagent), then it is a sign of antibody coating over the cells in vivo. It is imperative to mention that both IgG and IgM antibodies can be detected by using this test.
Techniques of DAT
- Take patient RBCs from an EDTA (ethylenediaminetetraacetic acid), which ensures the sample is anticoagulated.
- Dispense one drop of RBC suspension (2%-5%) separately into each of the 4 test tubes, and label the 4 tubes with tags: Poly, Control, anti-IgG, and anti-C3.
- Wash the RBCs with saline, and then tilt the tube upside down to decant the saline. Then clear the bottoms of the tubes with the left saline, and repeat this for 3 to 4 times. Dry the tubes with an absorbent wipe.
- Add two drops of polyspecific AHG into the "Poly" tube, and dispense two drops of 6% BSA to the "Control" tube.
- Shake gently to combine the contents in tubes, and RBCs in each tube will form a pellet or a button which will get tested for agglutination. Record the results.
- If the polyspecific reagent shows positive results, specific tests with anti-IgG anti-C3 reagents will be needed to identify the cell coating, whether it is antibody or complement or both.
- Dispense 2 drops of anti-IgG AHG to the "anti-IgG" tube, and 2 drops of anti-C3 AHG to the "anti-C3" tube. Shake to combine the content.
- The test needs to be very sensitive so we will have to incubate all the negatives for 5 minutes for enhanced coating. To detect weakness in coating, observe all negatives with microscope.
- If red top tube has been used for collecting sample, then false positive results might come.
- When clotting happens or it cools down, it is due to weakness in cold-acting auto-antibodies including anti-I, the condition takes place in In-Vitro complement.
- Avoid lavender-top tube for tying up calcium and magnesium ions.
- Avoid activation of complement in vitro.
10. In case of positive DAT, get following information on patient:
- Diagnosis of certain diseases
- Appropriate medication
- History of transfusion of RBCs and components of plasma
- Other tests that indicate destruction in RBCs
For more information about the DAT and IAT, watch the video below:
How to Interpret the Test Results
We know that antibodies attach to RBCs when DAT is positive. The extent of positivity depends on the strength of DAT and at the same time the amount of bound antibodies. But if the RBCs are destroyed already, this situation does not always relate to the severity. In direct antiglobulin test, antibodies are detected without identifying the cause and type of hemolytic anemia. To find out the reasons behind it, medical history needs to be observed and medical examination has to be conducted, for example, history of transfusion, drug reaction, etc.
It is important to mention that a small segment of population tests DAT positive without experiencing or manifesting any signs of hemolytic anemia. If DAT is negative, it suggests that antibodies are not attached to RBCs. Therefore, other causes can be detected and investigated.
Some situations in which DAT is positive are:
- Autoimmune hemolytic anemia (due to hyperactivity of immune system against RBCs)
- Development of antibodies on RBCs, the condition is called "drug toxicity". It is caused by some drugs that include cephalosporins, levopoda, dapsone, nitrofurantion, NSAIDs like ibuprofen
- When the donated blood is attacked by the immune system (as part of transfusion reaction)
- The blood types of mother and infant are different
- Leukemia including chronic lymphocytic leukemia
- An autoimmune problem called lupus
- Mononucleosis
- Syphilis
- Mycoplasma infection.
Sometimes the results of direct antiglobulin test can be impossible even without any disease or risk. Besides, the test can be interrupted by some drugs and some can cause the results positive without having hemolytic anemia. Some drugs that might cause hemolytic anemia are:
- Some antibiotics
- Insulin
- Some particular blood pressure medicines
