The endometrium is the inner lining of the uterus. Its thickness varies with a woman’s age, reproductive stage and specific point of her menstrual cycle. A thickened endometrium may or may not be a normal finding, depending on various factors of a woman’s menstrual stage. To evaluate endometrial thickening, ultrasound or magnetic resonance imaging (MRI) may be used.
Normal Endometrial Thickness in Menstrual Cycle
The endometrium normally changes in thickness and appearance throughout your menstrual cycle. These changes are associated with the hormonal changes that occur during the cycle.
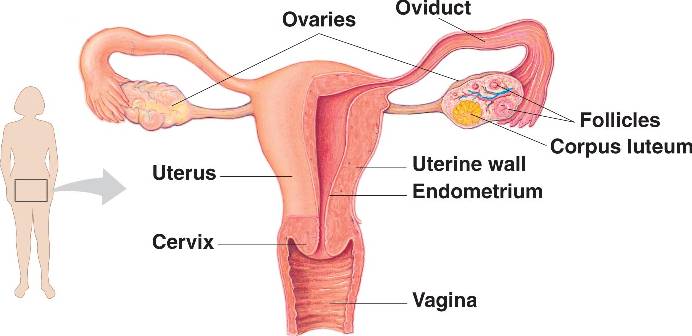
Early in the menstrual cycle, estrogen, which is produced by the ovaries, causes the uterine lining to grow, to prepare the uterus for possible pregnancy.
At mid-cycle, the ovary releases an egg during ovulation. Following ovulation, another hormone (progesterone) begins to increase to prepare the endometrium for implantation of fertilized egg. You may have endometrium thickening at this point. However, if fertilization does not occur, hormone levels decrease, triggering menstruation, which is due to the shedding of the uterine lining. Once completed, a new cycle begins.
What Causes Thickened Endometrium?
In most cases, endometrium thickening is non-cancerous (benign). Aside from the normal changes associated with the menstrual cycle, hormonal changes during perimenopausal stage may also cause endometrial thickening. Chronic disorders like obesity, diabetes, or PCOS (polycystic ovarian syndrome) may also be associated with thick endometrium.Aside from these, endometrial hyperplasia may also be associated with uterine cancer.
Symptoms of endometrial thickening include unusual changes in the length of menstrual periods, heavier menstrual blood flow, abnormal bleeding/spotting between periods, or postmenopausal bleeding. Anemia (low blood count) may also occur.
Risk factors associated with endometrial thickening include:
- Age > 35 years
- Racial factors: White women are more likely to be affected
- Women who have never been pregnant are more likely to have thick endometrium
- Reaching menopause at an older age increases your risk.
- Early menarche (when menstruation began)
- Obesity is usually associated with thick endometrium.
- Medical conditions such as diabetes, gallbladder disease, thyroid disease, or polycystic ovary syndrome
- Cigarette smokingincreases your risk.
- Family history of uterine cancer,ovarian cancer, or colon cancer
Can It Be Cancer?
If you are postmenopausal and you have an abnormally thickened endometrium, you will need further evaluation to find out if you are at risk for endometrial cancer. The endometrial thickening often reflects estrogen stimulation, which may be due to hormone replacement therapy or from intake of breast cancer drug, tamoxifen, or continuous estrogen production resulting from obesity. A rare cause is ovarian tumor, which may be producing excess estrogen.
Endometrium thickening may cause bleeding after menopause, but even without bleeding, the possibility of endometrial cancer cannot be ruled out. Confirmation may be done using endometrial biopsy. Endometrial thickness must be evaluated together with endometrial morphology as well as risk factors for malignancy when considering endometrial sampling.
Thickened Endometrium Diagnosis
An ultrasound evaluation of the uterine lining may be used as a screening tool. During pelvic examination, biopsy of the endometrium may be taken after performingdilatation and curettage. Hysteroscopy may also be performed to find abnormal areas in the endometrium. It involves the use of a thin device into your uterus to examine and remove tissues.
Abnormally thick endometrium may occur for various reasons, which may or may not be pregnancy-related. Causes may also classified based on whether you are pre- or postmenopausal.
Pregnancy-Related Causes
- Early pregnancy (<5 weeks)
- Ectopic pregnancy
- Intra-uterine blood clot
- Molar pregnancy
- Recent delivery
- Endometritis
- Retained placenta
Non-pregnancy Related Causes
- Endometrial cancer
- Endometrial hyperplasia
- Endometrial polyp
- Tamoxifen-related changes
- Hormone replacement therapy
- Endometritis
- Ovarian tumours
How to Treat and Prevent Thickened Endometrium
- In most cases, treat of endometrial hyperplasia involves removal of uterine tissue through dilatation and curettage (D and C).
- Postmenopausal women who are taking replacement hormones causing recurrent endometrial thickening should discuss with their gynecologists options which include either supplementing their therapy with progesterone or stopping therapy.
- Premenopausal women who have thickened endometrial may take oral contraceptives or progesterone as prescribed to thin out their endometrial lining.
- Surgical removal of the uterus (hysterectomy) and other reproductive organs may be advised for some women, particularly those who are postmenopausal or women who are not planning to have children. This will reduce their risk of cancer when their condition does not respond to progesterone therapy.
- Endometrial thickening can also be treated with oral or injectable progestin. It may also be used as a vaginal creamorin an intrauterine device. However, progestin treatment may cause vaginal bleeding similar to menstrual bleeding.
What Can I Do to Prevent Endometrial Thickening?
To reduce your risk of thickened endometrium:
- Take progestin / progesteroneif you are taking estrogen after menopause.
- Take birth control pills containing estrogen and progestin if your menstrual periods are irregular.
- Lose weight if you are obese or overweight. This may also reduce your risk of endometrial cancer.
