Both osteopenia and osteoporosis start with "osteo" which means bone. Both diseases weaken the bones and are very common in women who are menopausal and postmenopausal. Actually, eighty percent of those found to have weak bones are women over 40. It is important to differentiate osteopenia from osteoporosis, so you can respond appropriately.
Osteopenia vs. Osteoporosis: Definition
Osteopenia
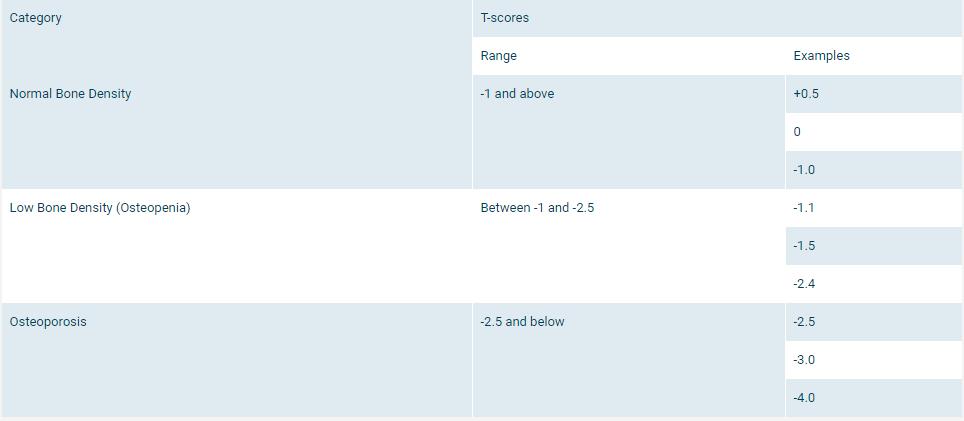
Osteopenia is the precursor to osteoporosis. If a person has osteopenia, he/she has a lower than normal bone density, but not so low as to be diagnosed with osteoporosis. When your bone density or T-score falls in the middle of -1.0 and -2.5, you have osteopenia. Osteopenia means a higher risk of osteoporosis, but osteopenia doesn't necessarily proceeds into osteoporosis.
Osteoporosis
If your bone mineral density is lower than -2.5, you will receive a diagnosis of osteoporosis. With this condition, your bones may be so weak that a bump, fall, bending over and even a cough can cause a fracture.
Osteopenia vs. Osteoporosis: Symptom
Osteopenia
Without a broken bone, the symptoms of osteopenia can be hard to identify. Often there is no pain or noticeable changes as your bones get thinner. But there is an increased risk to fractures as the bones lose their density.
Osteoporosis
Often, when the disease is in its early stages, a person won’t notice any symptoms. In later stages, it may cause loss of height and a dull ache in muscles and bones, particularly in neck and lower back.
During later stages of the disease, sharp pain can suddenly occur, usually accompanied by tenderness. It may go away in a short time or can linger as long as three months. This pain may not spread but could get worse when weight is placed on the area. Sometimes, bone fracture can occur without a fall or another trauma.
Diagnosis
When your physician thinks you may be at risk of either osteopenia or osteoporosis, he/she will ask you to take a bone density test. This will check for the density of bone in your spine, hip and wrist. This is painless, like an X-ray but with less radiation.
Your doctor might also recommend that you get an NTX blood or urine test. This is a test to measure the amount of bone you’ve lost. It will help your doctor have an idea about your bones to help with treatment choices.
Osteopenia vs. Osteoporosis: Treatment
Osteopenia
Treatment will be decided on an individualized basis considering bone health, and medical history and risk factors.
- One of the most recommended treatments for osteopenia is exercise. Exercise helps prevent falls and encourage bone growth. Both strengthening exercises and weight-bearing exercises are recommended.
- It’s important to commit to some lifestyle changes such as quitting smoking and limiting alcohol.
- Another thing to do is to supplement with vitamin D and calcium. To get the optimal dose, get your vitamin D measured with blood tests.
- Not all patients will need prescription meds. Your physician will assess your condition and decide the best course of treatment. Some medications that are used are zoledronate, ibandronate, risedronate, alendronate, and raloxifene.
Osteoporosis
In the comparison of osteopenia vs. osteoporosis, the treatment methods are different. The treatment options of osteoporosis include:
1. Medications
There are a few common drug treatments.
- Alendronate is usually taken once a week orally.
- Ibandronate can be taken once a month orally or as a shot four times yearly.
- Risedronate is available to be taken daily, weekly, bimonthly, or monthly.
- Zoledronic acid is taken through an IV every one or two years.
- Antibodies can slow bone reabsorption, maintaining bone density.
The medications can cause side effects in some people. Be sure to consult your doctor before taking any of these.
2. Hormone Therapy
Women who are postmenopausal are at a high risk for osteoporosis. Estrogen encourages stronger bones but it drops after menopause. Hormone therapy can be helpful as a treatment option in these cases. It isn’t often used as a first choice because it can increase your chance of:
- Blood clots
- Breast cancer
- A heart attack
- A stroke
A few hormone therapies include:
- SERMs or Selective Estrogen Receptor Modulators
- Thyrocalcitonin
- Parathyroid Hormone
3. Lifestyle Changes
Try to make sure you get plenty of vitamin D and calcium in your diet. Vitamin D is essential because it will help your body to absorb the calcium it needs. Try to eat:
- Dark, leafy greens
- Dairy products
- Enriched breads and grains
- Soy products
Cereal and orange juice generally have added calcium, so they are also great options. Also, make sure to quit smoking. Even a pack a day can decrease your bone density by as much as 5-10%.
4. Physical Activity
One of the first and most important things you can do is to get physical exercise. Whatever kind you can do will help to slow bone loss related to aging and improve your bone density. It can help with balance and posture, therefore lowering your risk of falls and injuries. The following activities can strengthen your spine, hips and legs.
- Strength training with weight machines, resistance bands or free weights
- Weight-bearing exercise such as walking or jogging
- Low-impact aerobics like elliptical training or biking
